Author Archives: jerseyshore
Hot Treatment vs. Cold Treatment – The Oldest Rivalry in Sports!

“Should I use heat or ice?” is the most common question I get in the office from patients, especially athletes, looking to ease their soreness after exercising. Commonly, there is a lot of confusion as to which method is best, when to use which treatment, and what separates the two. Fortunately, we have a guide to help you determine which treatment is best for you to get back in the game and doing what you love!
Why heat? Heat causes the small blood vessels in the muscle and surrounding tissues to dilate, increasing blood flow to the targeted area. This brings more oxygen and nutrients to the damaged tissue and removes harmful waste products. In addition, the heat can distract the nerves that carry pain signals, preventing their transmission to the brain for recognition. Finally, heat can also increase the pliability of the tissue, decreasing stiffness and spasms.
When to use heat: A simple rule to remember for heat treatment is to use it for chronic or old injuries. Here are a few examples:
- Low back pain
- Arthritic joints
- Trigger points/muscle spasms
As with everything, there are exceptions. For heat, one exception would be muscle soreness after a tough workout. A recent study shows that a simple over-the-counter heat wrap applied immediately after a workout with eight hours of low level heat can significantly decrease delayed onset muscle soreness (DOMS).
Why cold? Opposite to heat, cold treatments cause the small blood vessels to constrict, decreasing blood flow to the area. With new or overuse injuries, decreasing the blood flow helps to stop the body’s substances that cause redness and swelling commonly seen in these types of injuries. In addition, cold helps to numb the irritated nerve endings in the injured area.
When to use cold: Contrary to heat, cold is typically used for new, acute or overuse injuries. Here are a few examples:
- Ankle sprains
- Tennis elbow
- Achilles tendinitis
- Shoulder bursitis
While it is unclear whether ice actually helps the healing process, there is no doubt that it helps relieve pain. The most effective way to provide cold treatment to an affected area is to apply ice directly on the skin with an ice cup. However, it is important to keep the ice moving to prevent tissue damage. An additional method is using a freezer bag filled with ice cubes and a small amount of water, which can be easily molded to the area. A thin towel should be used also as a means of separation between the ice and skin. These treatments should be applied until the skin feels numb. One to three minutes with an ice cup and fifteen to twenty minutes with an ice bag should do the trick!
Sports and other means of exercise provide many opportunities for injury, both large and small. Proper management of these injuries using hot and cold treatments can help prevent further damage and get you back in the game! Have questions about an injury or need to be evaluated? Chat with us on Facebook, Twitter, or give us a call at 609-904-2565.
Tendonitis: Signs, Diagnosis and Treatments
What is Tendonitis?
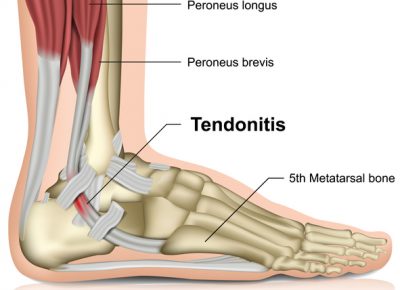
You may have heard tendonitis referred to as tennis elbow, jumper’s knee or golfer’s elbow. Despite the many nicknames that the condition has acquired, they all signify excessive inflammation of a tendon, which is the structure that connects muscle to bone. It is typically caused by overuse of the affected area, often from a repetitive activity or in some cases by a minor trauma.
Signs of Tendonitis:
- Intermittent pain at the site of the tendon
- Pain during movement or extreme pain in severe cases
- Stiffness, swelling or tenderness at the site of the tendon
- In severe cases, redness and swelling at the site of the tendon
- Patients often report starting a new high-volume activity prior to the onset of pain
Diagnosis:
Typically, imaging is not needed to diagnose tendonitis. However, X-rays may be helpful in older patients to help differentiate between tendonitis and degenerative joint disease, which can present with similar symptoms. In more severe cases of tendonitis, weakness or limited motion may require an MRI to rule out a partial or complete tear of the tendon.
Treatment:
Treatment is initially focused on reducing pain. Rest, ice and over-the-counter anti-inflammatory medications are common treatments, often tried by patients before seeing a doctor. However, a higher dose of oral or topical anti-inflammatories, braces and corticosteroid injections are typically prescribed at an initial visit with us. Once the pain is under control, our focus shifts to preventing the pain from coming back. Physical therapy, Active Release Technique and activity modifications are some ways that Jersey Shore Sports Medicine can help you prevent pain from returning – all without surgery!
Severe Cases:
Tendonitis that lasts longer than a few months can lead to chronic damage to the tendon, called tendinosis. Initial treatment is the same, but resolution of the symptoms often takes longer. If typical conservative treatments don’t do the trick, Jersey Shore Sports Medicine offers regenerative treatments, surgery-free, such as platelet rich plasma (PRP) injections and stem cell injections.
Tendonitis is a very common injury that can occur in active individuals. Early treatment is key to reducing pain and keeping you in tip-top shape! Have questions about tendonitis treatment or PRP? Chat with us on Facebook, Twitter, or give us a call at 609-904-2565.
What is a cortisone shot?

“Just get a cortisone shot”. That is the answer most people either give or receive in response to a complaint of pain somewhere in the body. However, not many people outside of the medical field actually know what a cortisone shot is, how it works, what it treats or how safe it is. In addition, there is a lot of bad information floating around out there that you have probably heard at some point. I am going to take a few minutes and explain what a cortisone shot is and who should get one.
Cortisone is hormone produced naturally in the body by the adrenal glands. However, it is better known for its uses when produced synthetically. Cortisone is one of many options is a class of medications called corticosteroids. But since it has been around the longest, its name is used in a generic fashion to represent the entire class of medications (like Band-Aids for adhesive bandages).
Corticosteroids are very strong anti-inflammatory medications. Inflammation is the body’s way of removing foreign substances, like bacteria and viruses. It is also the way the body heals damaged tissue, like a sprained ankle. However, sometimes the body’s inflammatory response is too strong, leading to persistent pain, such as with tendinitis. Corticosteroids can decrease or stop this excess inflammation, reducing or completely relieving the pain
Corticosteroids can be given in an IV, as a pill, as a cream or as an injection. In sports medicine, we most frequently inject the medication directly into the area of inflammation. It is most effective in treating tendinitis, bursitis and arthritis. Some common examples are tennis elbow, rotator cuff tendinitis, hip bursitis and knee arthritis. There are a few structures that should not be injected due to fear of rupture, and they include the patella and Achilles tendons.
Corticosteroid injections are very well tolerated. However, there are a few potential side effects. A couple of the more common ones include, redness of the face or around the injection site. They are harmless and go away in a few days. There is always the risk of an allergic reaction. Diabetics have to be very careful, as corticosteroids can cause the blood sugar levels to spike as high as 500-600 for a few days. Multiple injections in the same area can cause the tissue under the skin to breakdown leaving a large dimple; or the skin can lose its color leaving a pale spot. Patients that are on blood thinners can safely get a corticosteroid injection.
The most common question/fear asked by patients involves the long-term safety of these injections. The answer is that if utilized properly and judiciously, they are extremely safe. Injections can be given to an individual joint or structure 3-4 times per year, or once every 3-4 months. Injections to different body parts can be given at the same time. There is some concern that injections done more frequently may cause deterioration of the cartilage or tendons.
Cortisone injections are an excellent treatment option for sports medicine doctors. They provide rapid relief of pain, allowing the patient to return to work and/or activity quickly. They also provide the relief of pain often necessary to allow the patient to perform the rehabilitation needed to correct the underlying cause of the pain. I use them frequently in my office and find them to be a safe and effective treatment for many musculoskeletal injuries.
Plantaris-The unknown muscle of the calf

“It felt like I got kicked in the back of the leg” is one of the scariest phrases for athletes. When that feeling occurs in the heel it usually means the Achilles tendon has ruptured. Oftentimes that means surgery, though there is literature that says surgical repair may not be necessary; but either way, the athlete is facing a long rehabilitation.
However, that same feeling can also be felt higher up in the calf. When that happens, the athlete can see significant swelling, pain and sometimes bruising. When they present to the office, they often believe they tore one of the 2 large muscles of the calf, the gastrocnemius or soleus. However, there is a 3rd, small and often unknown muscle of the calf that is more frequently the culprit, the plantaris.
The plantaris muscle starts from the bottom of the thigh bone (femur) and runs behind the knee into the top portion of the calf. The tendon then runs the rest of the way down the calf and attaches to the heel next to the Achilles tendon. Often the rupture is located where tendon and muscle attach, which is why the sensation is felt in the middle of the calf and there isn’t much bruising. If the tear is higher up in the muscle belly, there will be significant swelling too.
If the tendon tears, then doesn’t it have to be fixed like the Achilles or rotator cuff? The answer is no. The plantaris provides no significant contribution to the functions of the other muscles in the calf, which are pointing the foot down towards the ground and flexing the knee. There is some belief that it has some other roles in the movements of the lower leg, but again, nothing vital. Therefore, treatment involves relieving the immediate symptoms of pain and swelling, then regaining the strength and ROM of the calf muscles with therapy.
Calf injuries can be very scary as the first thoughts often go towards the Achilles tendon and surgery. However, when the location of the injury is higher up, the structure commonly damaged is the plantaris. When that is the case, with accurate diagnosis and good therapy, the athlete can return to previous levels of activity and performance without surgery.
Why Does My Knee Hurt?

“It hurts when I squat.” “It hurts when I sit for a long time, like long car rides.” “It hurts when I walk downstairs.” If these statements sound familiar, you’re not alone.
They are the most common symptoms for a widespread knee problem, patellafemoral pain syndrome (PFPS). PFPS is a generic term that encompasses many different causes of pain in the front part of the knee, particularly under the kneecap (patella). It can be found in all ages and across the spectrum of activity levels, but is most commonly associated with teenage and young adult female athletes.
PFPS is most frequently caused by abnormal tracking of the kneecap. The patella sits in a groove at the far end of the thigh bone (femur). As you flex and straighten your knee, the patella glides up and down through this groove. A number of structures assist in making sure the patella stays in proper alignment. These include the smooth cartilage that lines the end of the femur and undersurface of the patella, called the articular cartilage. The muscles and tendons of the thigh and hip also play an important role. And finally, the alignment of the bones above and blow the knee are important.
Some of the underlying causes of PFPS occur because of natural growth and development. For example, as girls go through puberty, one of the natural changes is widening of the hips. Sometimes this widening causes change in the way the muscles and other tissue pull on the knee and patella, leading to abnormal tracking. This is one of the reasons PFPS is so common in adolescents and young adults. Another common structural abnormality is flat feet. When you walk with flat feet, your foot turns in more, and that can lead to changes in patella tracking, and ultimately knee pain.
In other cases, PFPS is completely our own doing. The most common example of that is simple overuse. Athletes that drastically increase their activity, especially running and jumping, are at risk for developing PFPS. In addition, if an athlete’s training program is not well balanced, the muscles in the thigh and hip can develop imbalances. These imbalances can lead to abnormal forces pulling at the patella leading to improper tracking. This is extremely common as many basic workouts focus primarily on the largest muscle groups of the legs and ignore the smaller stabilizing muscles that help maintain proper movement, including patella tracking.
There are a number of factors that can contribute to pain in the front of the knee. All of them must be evaluated to obtain an accurate diagnosis. And once identified, all abnormalities must be properly addressed, whether with physical therapy, braces orthotics, etc. to fully resolve the pain long-term.
